STEPS
.png)
project type
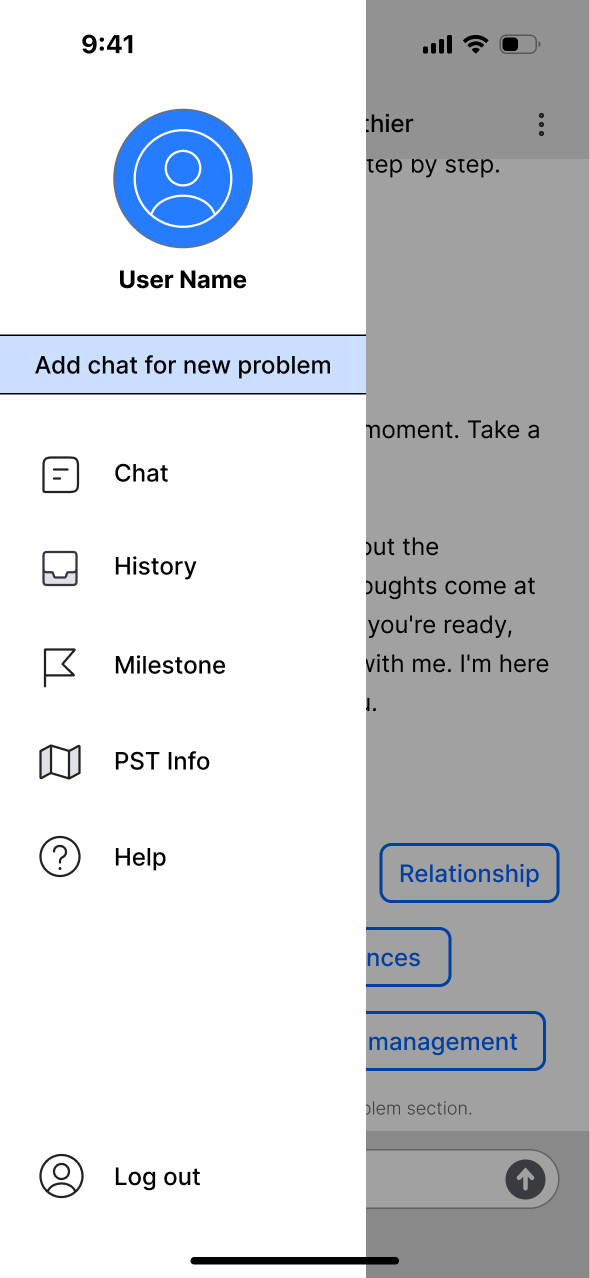
This project aims to develop problem-solving training (PST) for civilians, veterans, and service members with Traumatic Brain Injuries (TBI). In collaboration with a study at TIRR Memorial Hermann, it focuses on creating an e-health app to improve accessibility.
I designed a chatbot app that integrates the original phone- and paper-based training, enhancing emotional support, organization, and conversation flow for easier access to PST, which helps improve psychological health after TBI.





















.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
